ѪҺ�ڿ����ĵ���ƪ���������в㻼�ߵ���ϼ��ڿ�����̽��
����ժҪ��Ŀ�� �����������в���ٴ���ϡ����� ���ѡȡ2008��1��2018��1������ԺסԺ���Ƶ�30���������в㻼��, ����X����Ƭ���ĵ�ͼ���30��, CTѪ����Ӱ���26��, ������ǻ����Ӱ4�������л��߽����ڿ�����, ͨ��ֹʹ�����Լ���ѹ�ȷ�������, ʹѪѹ����Ϊ100110/6070mm Hg����� ͨ���Ի��߽�����ϸ�������Լ������, ҽʦ���������������, ʵ���Ҽ����, 30���������в㻼����, X��ȷ��Ϊ30.0%, ECGȷ��Ϊ0, CT��������ǻ����Ӱ���ȷ��Ϊ100.0%��������ʹ֢״��27������, ͨ��ֹʹ�Լ������ƺ�, ��6h��ʹ֢״�����Ի������ʧ;26���ϲ���Ѫѹ����, ͨ����ѹ���ƺ�, 21�������������в�����ȶ�����ת, �Ѿ���Ժ;1���ϲ�����˥�����ڼ������в�������;1������ȷ���תԺ�����мв�����, ������Ч������4���Ǹ�Ѫѹ������, ͨ��ֹʹ���ȷ������ƺ�, ��������õ��ȶ�����ת, �Ѿ���Ժ������ ҽʦ���Ը��ݻ��ߵ��ٴ������Լ�֢״�����������, �����������Ϊ�������в�Ļ���, ���Խ���X����Ƭ�Լ��ĵ�ͼ������ҽʦ���, ���нϺõ�ɸѡ����, ����CTѪ����Ӱ����нϸߵ���Ϸ�����, �ȽϿɿ�, �������в�����Ӧ�ó����Ķ�ͼ���ʮ�ֹؼ�, ������ó�����������ǻ����Ӱ�����ܹ�����ҽʦ��һ��ȷ�
�����ؼ��ʣ��������в�; ���; �ڿ�����;
����Clinical analysis of aortic dissection
����DOU Zhemin YE Dan DENG Yiming
����Beijing Aerospace General Hospital Beijing Tiantan Hospital Affiliated to Capital University of Medical Sciences
����Abstract��Objective To analyze the clinical diagnosis of aortic dissection. Methods Thirty cases of aortic dissection were randomly selected from January 2008 to January 2018 in our hospital, including X-ray chest, 30 cases of electrocardiogram, 26 cases of CT angiography, 4 cases of aorta angiography.All patients were treated with internal medicine and treated with pain relief, sedation and hypotension, and the blood pressure was reduced to 100-110/60-70 mm Hg. Results The patients with detailed interrogation and examination, the doctor can make a preliminary diagnosis, laboratory examination, 30 patients with aortic dissection, X-ray accuracy is 30.0%, ECG accuracy is 0, CT, the aortic lumen imaging diagnostic accuracy was 100.0%.In the 27 patients with pain symptoms, the pain symptoms of 6 h were significantly alleviated or disappeared after the pain and sedative treatment.In 26 patients with hypertension, the aortic dissection of 21 patients was basically stable and improved after the treatment of hypotension. 1 case of patients with heart failure died during the examination;In one patient, the intercalation was ruptured and the patient died.In 4 cases of non-hypertensive patients, after treatment with analgesic and sedation, the condition was basically stable and improved, and discharged. Conclusion physicians may, according to a tentative diagnosis of the patient's clinical signs and symptoms in patients with difficult to diagnosis main artery dissection, can help doctors diagnose X-ray chest X-ray and electrocardiogram (ecg) checks, has better screening effect, the diagnostic accordance rate of CT angiography have higher, more reliable, aortic dissection of the early application of echocardiography is critical, in addition with ultrasonic and aortic lumen imaging examination can help doctors confirmed further.
�����������в��²����ؽ϶�, �����Ϊ��Ѫѹ����������Ӳ���������ۺ�����, ����Ҫ������Ĥ˺��, �Ĥ�²��ܵ�ǿ��ѪҺ���, �Ӷ�������Ĥ������չ����������, �������ڶ������γ��桢����ǻ, ����ͨ�������˺�����ľ�����ʹ, ��δ��ʱ��Ԥ����, ����в��������[1,2]����������ʾ, δ�õ���ʱ��ǡ�����ƵĻ���, ��3%�Ļ���ֱ�����, 37%~50%�Ļ��߲���2d������, 60%~70%�Ļ��߲���1��������[3]����һ���㡢��Ч����Ϸ�ʽ��Ϊ�������в��ٴ������ṩ���ݡ��ع��Է�����Ժ2008��1��~2018��1������ԺסԺ���Ƶ�30���������в㻼��, ͨ����ϼ��ڿ�����ȡ���˽Ϻõ��ٴ���Ч, �ֱ������¡�
������1 ������������������ (����)
��
����1 �����뷽��
����1.1 һ������
�������ѡȡ2017��1��~2018��1������ԺסԺ���Ƶ�30���������в㻼��, ����, ��21��, Ů9��;����18~71��, ƽ�� (50.7±11.4) �ꡣ����:26����Ѫѹ, ����, �ϲ����IJ�7��, �ϲ�����13��, 5�������ۺ���, 3����֢, 1��������������խ, 1����Դ����ס��ٴ�����:22����ʹ, 14����ʹ, 11����ʹ�鸹ʹ, 8��������ʹ, 6��������ʹ�鸹ʹ, 3��δ����������ʹ;7��������, 5�������������, 4����֫��������, 2��Ż��, 2��ͷ��, 1��һ���������߲��Գơ����ݹ���Debakey�����з���:21�����͡�7�������Լ�2�����͡�
����1.2 ��Ϸ���
�������л����Ƚ����������Լ�������, ����, X����Ƭ���ĵ�ͼ (ECG) ���30��, CTѪ����Ӱ26��, �����Ķ�ͼ (UCG) ���4��, ������ǻ����Ӱ4����
����1.3 �ڿ�����
�������л��߽����ڿ�����, ͨ��ֹʹ�����Լ���ѹ�ȷ�������, ����, ֹʹ������ѡ����ȡ���ڼ���䶡�Լ�������ҩ��;��ѹ����ѡ��50mg�����ֿ�Ƭ��, 2��/d, ����ȡ������͡������ƻ���ѹ�����Ⱦ���ע��, ��6h��ʹ���ߵ�Ѫѹ����Ϊ100~110/60~70mm Hg (1mm Hg=0.133k Pa) , ������Ѫѹ����Ҫ������ҩ�ļ���, ����5~7d, ������ACEI��������Լ�������������ҩ��, ����סԺ�ڼ��Լ���Ժ֮����Ҫ���ڱ���Ѫѹ���ȶ�;δ�ﵽ��Ѫѹ�Ļ�����Ҫ�������н�ѹ���ơ�
����2 ���
����2.1 ���������������������
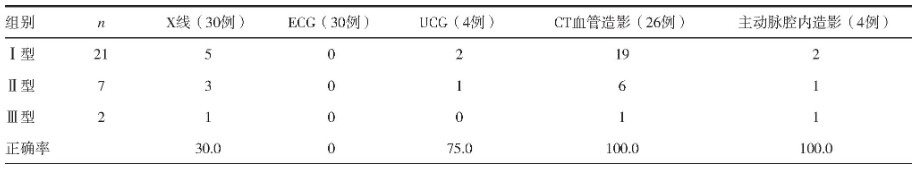
����30���������в㻼����, X��ȷ��Ϊ30.0%, ECGȷ��Ϊ0, CT��������ǻ����Ӱ���ȷ��Ϊ100.0%������1��
����2.2 �ڿ����Ƶ��ٴ�Ч��
����������ʹ֢״��27������, ͨ��ֹʹ�Լ������ƺ�, ��6h��ʹ֢״�����Ի������ʧ;26���ϲ���Ѫѹ����, ͨ����ѹ���ƺ�, ��6h��Ѫѹ����Ϊ100~110/60~70mm Hg;21�������������в�����ȶ�����ת, �Ѿ���Ժ;1���ϲ�����˥�����ڼ������в�������;1������ȷ���תԺ�����мв�����, ������Ч������4���Ǹ�Ѫѹ������, ��3�����ߵ�Ѫѹ����100~110/60~70mm Hg, ͨ��ֹʹ�����Լ���ѹ�ȷ������ƺ�, ��������õ��ȶ�����ת, �Ѿ���Ժ, 1��δ����100~110/60~70mm Hg�Ļ���, ͨ��ֹʹ�Լ������ƺ�, ��������õ��ȶ�����ת, �Ѿ���Ժ��
����3 ����
���������в�������Ĥ�ֲ�˺��, ���ܵ�ѪҺ��ǿ�����, ʹ��Ĥ��һ���������չ, ���¶����ڳ����桢����ǻ[4]���������в���Ҫ�������ˡ������������Ӳ������Ѫѹ����, ���з��������Ը�Ѫѹ��Ϊ����, ���ٴ����ֶ�����, ���������Ϊѹ��Ѫ�ܡ��ر���������ʹ��, ����Ҫ��������������֧�ܵ�ѹ��, �Ӷ�����ȱѪ����[5,6]���������в㶯�������ټ�, ������ÿ��ÿ�����˿�Լ5~10��, �߷�������50~70��, ��ȴ��һ�ּ������յ���Ѫ�ܼ���, ����65%~70%�Ļ����ڼ�������������ѹ��������ʧ���ȡ�����ϲ�֢��δ��ʱ��Ԥ, ��Σ����������, �����༲�������ϼ�, ����������֢״, ��������»��ߴ����������ʱ��, �Դ�Ӧ���ڸ��軼�߽������, �Ӷ������ٴ�����[7]�������ٴ��ϳ�ʹ��CT���, �����ȷ���߲���̶�, �����жϻ�����������֧����, Ϊ���ֲ�CT��ϲ���֮��, �ٴ�ѧ�߳����Ž���ɫ�����ճ���Ӧ�����ٴ�, ���֤ʵ, �����Ч������[8,9]��
���������о���, 30���������в㻼����, X��ȷ��Ϊ30.0%, ECGȷ��Ϊ0, CT��������ǻ����Ӱ���ȷ��Ϊ100.0%, CTѪ����Ӱ�ܹ������ع��Լ�������Ӱ��, ��������ʾ�ضμв��ͼ��, �ܹ�ȷ��Ϣ����������в�, ͬʱ���������в㸽��Ѫ˨�����������, ���Dz������ڴ��߽��м��[10];����������ǻ����Ӱ�����ϵ���ȷ��Ϊ100.00%, �����߱������ŵ�, �����ܹ��۲쵽�����в�ij������, ȷ���������в�ķ�Χ��ǻ�ڵ�Ѫ���ٶ��Լ����ߵIJ���̶�, ������Ҫ�����������ƵĻ���ʮ����Ҫ, ���Ƕ�ҽ����Ա�нϸߵļ���Ҫ��, ��Ҫ��������Ѫ�ܽ��뼼����
�����ڿ�������Ҫ��ֹʹ�����Լ���ѹ�ȷ���, ����������Ѫ�Լ�����ѹ���ٶ�, ��������������ڵĴ̼�����ר����Ϊ���������������ǿ, ��ֱ����ʹ�������в��������, ���, ���ۻ������������ѹ��λ����Ƿ������ʹ��Ӧ�ò����������ͼ�, ���������ҵ���Ѫ�ٶ�, �����������в���������������[11]��
������������, AD�DZȽ��ټ����кܸ߲����ʵ�һ����Ѫ�ܼ���, �������в��֢״������ͬ, �Ը�ʹΪ��Ҫ���ֵ��������в㻼��, ���Ը�ʹ��������Ժ, ������Ϊ���������ס����Ե���������ϵͳ����, �����ԭ��: (1) ˼ά����:����ҽʦ��AD����ʶ����, ������ȷ����, ���ڳ��ָ�ʹ֢״ʱ�����dz��������� (2) AD�ٴ����ָ���, ȱ��������, ����ʹ����ʹ���, Ҳ���Ա���Ϊ��ʹ�����ʡ��������귵��������������ʧ���ݿˡ�����˥�ߡ���ϵͳ֢״��, �ʸ���ϴ�������; (3) �������ٶ�, ������, �漰ѧ�ƹ㡣�ڡ��⡢������Ⱦ����ר�Ƽ�������������ʹ����ѯ�ʲ�ʷ�����岻��ϸ[12]�� (4) δ��ȡ��ȷ��ҽ�����:���ڸ�ʹʹ���߽��и���B�����, ��δ���ǽ�һ���и�����ǿCT��顣 (5) �����������AD��ϵĽ��������CT��ǿɨ����Ѫ���ؽ�������MRI[13,14,15], ����ҽԺ������Դ����, 8Сʱ����������ǿCT��Ѫ���ؽ�����, ����MRI, ����������ѡ�
���������
����[1]Τ����, ��ѧ��, ������, ��.�������в���������[J].�й�ҽҩָ��, 2012, 10 (26) :136-137.
����[2]��С��, �����, �½���.�������в��ٴ��ص����[J].ʵ�����Է�Ѫ�ܲ���־, 2012, 20 (4) :607-608.
����[3]Howard DP, Banerjee A, Fairhead JF, et al.Populationbased study of incidence and outcome of acute aortic dissection and premorbid risk factor control:10-year results from the Oxford Vascular Study[J].Circulation, 2013, 127 (20) :2031-2037.
����[4]�����, �ֹ�Ϊ.ʵ���ڿ�ѧ[M].��13��, ����:��������������, 2009:1656-1659.
����[5]���ϼ, ֣�ǰ�, �����.�����������в�����Ϊ�����ļ������ٴ�����[J].�й�ȫ��ҽѧ, 2012, 15 (12) :1380-1382.
����[6]����, ��˼��, ��άѫ, ��.�����������в��ٴ������ķ���[J].�й�ѭ֤��Ѫ��ҽѧ��־, 2013, 5 (6) :588-592.
����[7]Michael EB, Natalia NE, Alan JM, et al.Propensity Score-Matched Analysis of Open Surgical and Endovascular Repair for Type B Aortic Dissection[J].Int J Vasc Med, 2011, 20 (11) :1-7.
����[8]������, ������, ��ԲԲ.�Ը�ʹ������Ϊ�����ֵļ����������в�����������[J].�ٴ���������, 2013, 26 (8) :11-14.
����[9]������, ����, ����, ��.64������CT���������в㶯������Ӧ�ü�ֵ[J].�й�Ѫ����ѧ��־, 2010, 20 (1) :149-151.
����[10]������.�˴Ź�������������в����ϼ�ֵ[J].ҽѧ������ʵ��, 2011, 20 (3) :320-321.
����[11]���۾�, ����Ȩ, ������.�������в���о���չ[J].��Ѫѹ��־, 2002, 10 (2) :915.
����[12]CHEN HZ.Utility medicine (edition 12) [M].Beijing:The People’s Publishing Company, 2005:1593-1597.
����[13]���, ����Ӣ, ����÷, ��.�������в������ԭ������ʩ̽��[J].ʵ�����Է�Ѫ�ܲ���־, 2005, 13 (6) :383.
����[14]����, ����, ����, ��.�������в�12������ԭ�����[J].�ٴ���������, 2013, 26 (10) :29-31.
����[15]����, κ����, �Ժ���, ��.�������в�����Ϊ������ͻ��֢һ��[J].�ٴ���������, 2013, 26 (3) :11-12.
����鿴>>ѪҺ�ڿ����ģ����㷶��8ƪ����������